The basics
Many people find that the skin on their abdomen becomes loose after pregnancies, significant weight loss, or through ageing.
Abdominal wall scars, including caesarean section scars, can become recessed, and the excess hanging skin is sometimes called an ‘apron’. This is uncomfortable, makes clothing choices difficult, and can lead to infections under the flap of skin. Once this excess skin is present, exercise, diet and a healthy weight – though important – are unlikely to correct the problem.
Abdominoplasty is the surgical procedure used to remove excess skin from the middle and lower abdomen, to remove fatty deposits through liposuction at the same time, and if necessary, tighten the muscles of the abdominal wall.
What can I expect to achieve?
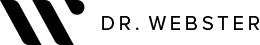
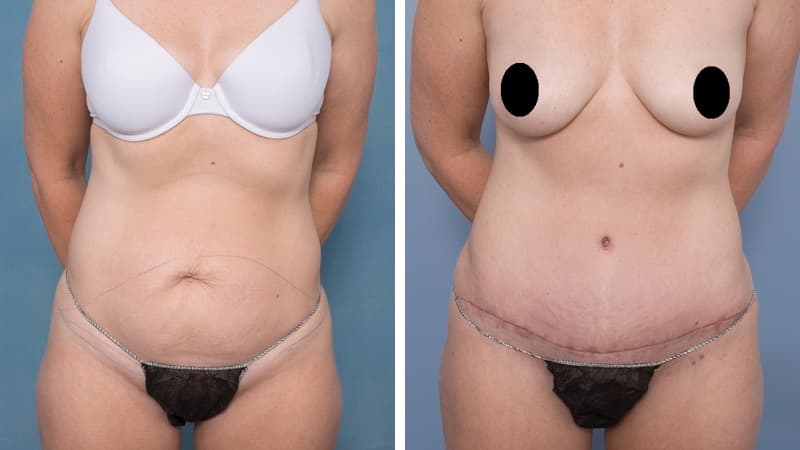
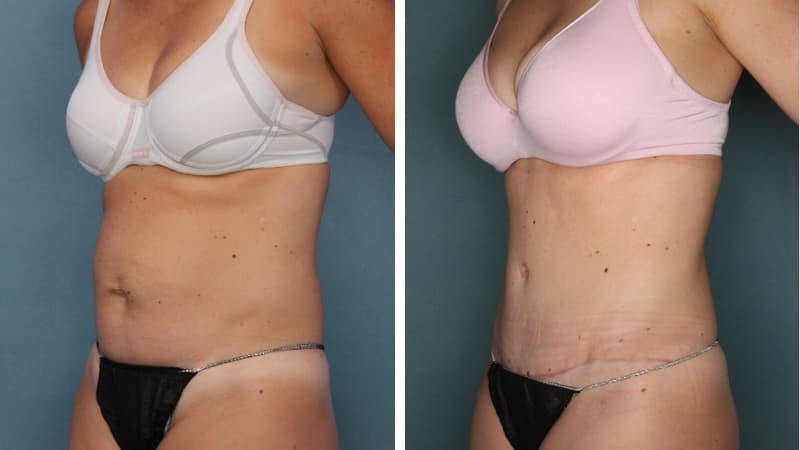
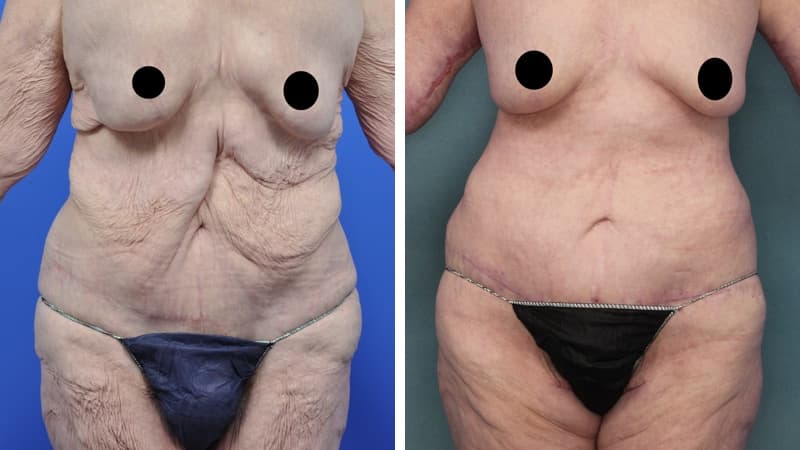
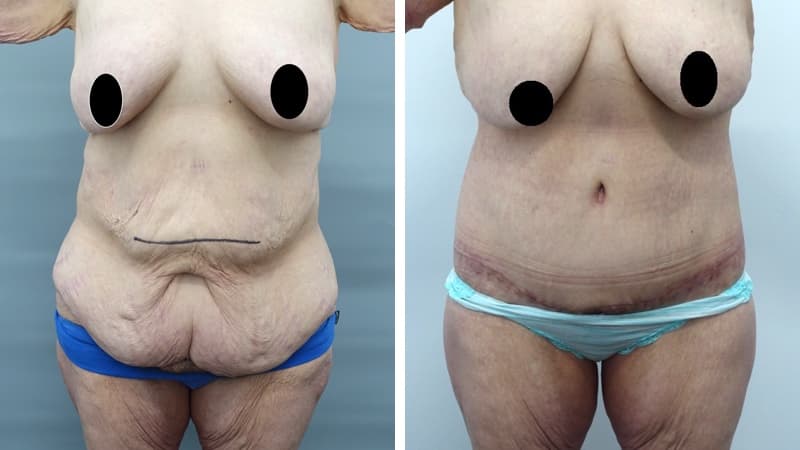
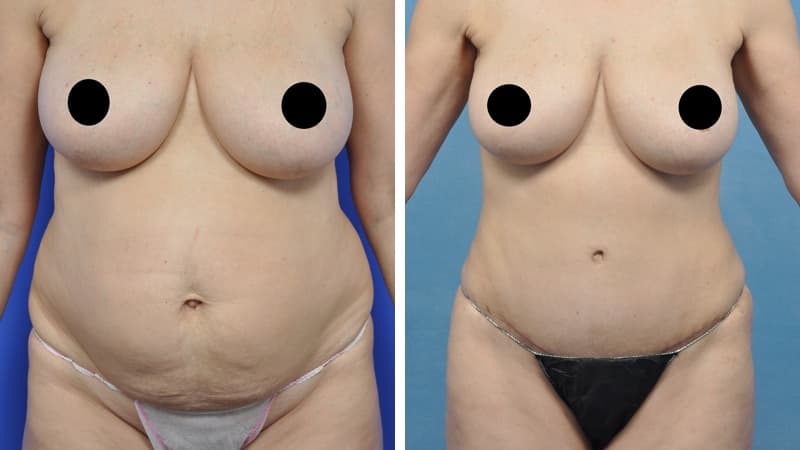
Abdominoplasty reduces a protruding or drooping abdomen and smooths loose skin. It can make a major difference to the body shape. Virtually all patients undergoing abdominoplasty feel very positive about its results.
Abdominoplasty is a very satisfying experience for most patients. It restores the abdominal wall shape, where diet and exercise cannot. It allows restoration of a pleasing body shape, and allows the patient to wear figure-hugging clothes if they wish.
Abdominoplasty is not a treatment for obesity. Excess hanging skin can make exercising difficult, so occasionally it is preferable to remove this before weight loss is attempted. In general, however, I advise overweight patients to lose weight before undergoing surgery.
The scar from an abdominoplasty is a low horizontal line just above the pubic area. Often a small circular scar around the navel will be necessary too. The patient’s shape determines the exact size and placement of the scar. It is often necessary to remove skin and fat from the flanks (love handles) and lower back to achieve the best result, and in this case the scar may go most or all of the way around to the back. Sometimes liposuction is used as well.
What happens before surgery?
I will explain the exact procedure and discuss with you which scar position and length will give you the best shape. You will be shown real pictures as part of the consultation, which may include pictures taken during surgery. This helps you to gain a realistic understanding of the procedure, and the results that can be achieved.
What happens during surgery?
Throughout your surgery, the team will be focused solely on your care. We will position you safely, keep you warm, and respect your dignity.
When you arrive at the hospital, you’ll be admitted to a pre-op room, where the nursing staff, the anaesthetist and I will meet you in turn. I’ll talk with you and mark you carefully. We’ll go over any questions you have.
Next, you’ll be transferred to the operating room. Your anaesthetist will carefully put you to sleep. You may remember entering the operating room but that is all you will know until you wake up in recovery. Once you are asleep, we will put in an IV and probably a urinary catheter, which will keep you comfortable and allow us to monitor your fluid status.
I will inject a large volume of dilute local anesthetic fluid into the area of the surgery. You will be fitted with monitoring equipment so that we can continuously check your vital signs.
The surgery will be performed extremely carefully. In most cases, pain pump catheters will be placed into the rectus sheath – these are attached to a pain pump which slowly drips local anaesthetic solution into the catheter to keep your rectus repair much more comfortable.
Dressings are applied to your wounds at the end of the procedure. Typically all the stitches are buried and dissolving.
You’ll wake up wearing a compression garment, with the IV and urinary catheters in, drain tubes from the wound, possibly a pain pump, an oxygen mask on and possibly a PCA – a patient controlled analgesia system. This sounds scarier than it is – it is routine practice after surgery and helps you recover. You’ll be able to talk freely, move around the bed and there will be someone with you at all times.
In the recovery room, a nurse will be stationed to sit with you. Once you’re fully awake, and with good vital signs and pain control, you’ll be transferred to your room in the ward.
Now the recovery process begins. Initially, we’ll let you rest and sleep, and monitor your pain and progress. The day after the surgery, we’ll begin to get you mobile.
What happens after surgery?
The hospital stay required after an abdominoplasty varies from one to four days, depending on the operation. If muscle repair is part of the operative plan, recovery is slower than if no muscle repair is needed.
Before the end of the operation, local anaesthetic is inserted into the wound area to minimise any discomfort on waking.
You will be closely monitored by the nursing staff postoperatively, and given all the pain medication you need. An IV drip will give you fluid, and initially you will have an oxygen mask. After the surgery, drain tubes may be required for several days to remove excess fluids from the wound. Your abdomen will be swollen for a few weeks after surgery and you will experience some discomfort. A urinary catheter may be necessary for a day or so.
The intravenous drip will be removed when you can drink well.
Possible complications
Complications of abdominoplasty include infection, haematoma and seroma (blood or fluid collections under the wound), wound breakdown requiring regular dressings, and a poor scar requiring minor revisional surgery. There is always some numbness of the skin just above the scar after this surgery. Please read the important document “Consequences, Risks and Complications of Abdominoplasty” which we will supply you with.
If you smoke, you must stop two weeks before surgery, and abstain for two weeks after surgery.